As originally published on reengineeringcancertreatment.com
Summary
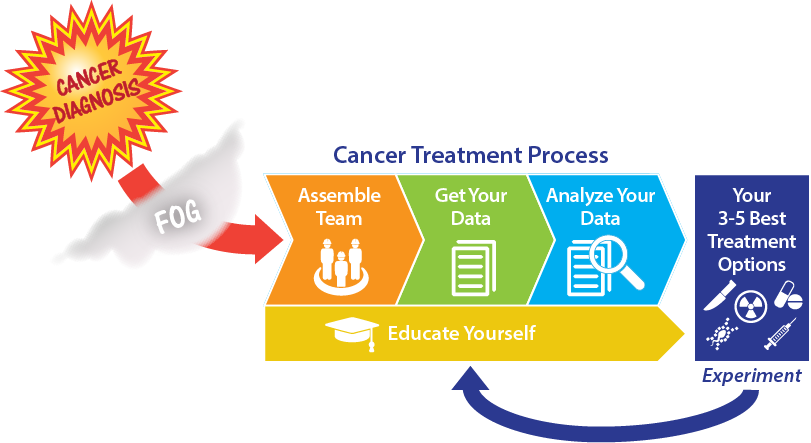
A cancer diagnosis can be shattering to an individual and his or her family and friends. The emotional earthquake can make everyone’s mind turn to mush. What does it mean? What do you do first? What are the right questions to ask? This article is intended to empower people confronted by a cancer diagnosis with an overview of the first steps in the treatment process to find their treatment options, updated to take into account the new possibilities offered by technologies for personalization of cancer treatment. In addition to establishing a support team and learning about your disease, treatment, and immediate steps, it’s important to get tests of the genetic profile of your disease and see if the latest targeted and immunotherapy treatments are options you should consider.
My Cancer Diagnosis
While on vacation in July of 2018 I started experiencing extreme belly pain. I couldn’t sleep. After a week, I decided to go to the emergency room to find out what the problem was. After getting a scan, a sober-faced emergency room physician told me, “You have lymphoma.” “Huh?” I thought. “That’s wasn’t on my list of possibilities.” I had expected to hear that I had gallstones, kidney stones, a hernia, or maybe a stomach virus. Pushing down a sea of emotions — disbelief, fear, anxiety — I asked, “What do I do next?” “You’re from Boston. You should find an oncologist at Dana-Farber or Mass General.” I got an appointment to see an oncologist who agreed to make space to see me as fast as possible.
The Shock of a Possible Death Sentence
The devastating shock of a cancer diagnosis confronts people with their mortality, and they can dip into depression. They are often scared, depressed, and anxious. The clock is ticking. It’s overwhelmingly complex. As Samuel Johnson said a few centuries ago: “Depend upon it, sir, when a man knows he is to be hanged in a fortnight, it concentrates his mind wonderfully.”
Immediate Needs: Social Support and Information
The challenge for people with a cancer diagnosis and their loved ones isn’t finding an explanation of their disease or a perfect checklist for their treatment — it’s about how to get through the fog of their emotional upheaval to think coherently and operate in a focused way. The steps for cancer treatment aren’t hard to find. People usually get stacks of information from their physician’s office when they are diagnosed. And there are a number of online guides for people with a cancer diagnosis. For example, CancerCare.com is an especially good resource for materials aimed at a variety of audiences. The best way to get through the fog of a cancer diagnosis is to walk through the treatment process with someone who understands the system (e.g., patient navigators) or those who have “been there” (survivors), who can listen, answer questions, and probe/guide in a gentle and helpful way.
Step One: Assemble your team of family, friends, and medical experts to clear the fog and for peace of mind, hope, love, encouragement, and support for day-to-day living. Here is a checklist:
- Consider getting help to process your emotions and for your mental health, such as a therapist or meditation coach, and keep exercising to help clear your head and keep a positive mental attitude. Friends recommended meditation and mindfulness to me, so I tried a group session and some free guided meditation apps, which helped me learn how to relax.
- Build and expand your trusted team of medical professionals, including a primary care physician, oncologist, and dietician, and others who can help with other aspects of your overall health, such as a fitness coach, physical therapist, or friend to keep you active. I tried an acupuncturist who brings Eastern approaches that I feel were part of my smooth sailing through chemotherapy.
- Choose someone to accompany you to appointments to provide a second set of ears. You or they should take notes, keep them in a filing system, and you should consider recording conversations. It’s a bonus if they have experience in navigating the health system.
- Set up a system for communicating with friends, family, and your co-workers. This can be an email distribution list, or you can use a website or app (e.g., Facebook, Instagram, CaringBridge, PostHope). When in doubt, you should lean in to communicate more. I knew it was time to send another group message when I started receiving individual messages asking how I was doing.
- Make arrangements to cover day-to-day life on the home front, such as meals, errands, childcare, and driving to appointments. And consider your financial and legal administration, such as insurance, bills, and debt.
Step Two: Educate yourself about your disease, treatment, and immediate steps. You will want to gather as much information as you can absorb. It can be overwhelming, and well-meaning and caring friends will tell you about treatments you’ve never heard of. In the end you have to make informed decisions, relying on your team of health professionals. Here’s a checklist:
- Search online on reputable sources of general medical advice, e.g., Google, WebMD, Mayo Clinic, Cleveland Clinic; cancer groups, e.g., the American Cancer Society for patients and families has answers to frequently asked questions after a diagnosis, as does the National Comprehensive Cancer Network (NCCN); and groups for specific cancers, e.g., the Leukemia and Lymphoma Society. To go really deep, the latest medical therapies and tests are presented at medical conferences, such as ASCO and ESMO. To distinguish between good, evidence-based information and hokey ideas and scary diagnoses, you may want to find someone trained in this kind of research, such as a health sciences librarian at your nearest academic medical center.
- Find people who have been through this, e.g., through online forums, such as PatientsLikeMe, or PatientPower, or support groups in your community, such as Gilda’s Club, or read blogs and books from reputable sources. Many people have generously shared their lessons on what to do for those who might follow them, such as Bryce Olson, who advocates getting sequenced; and Glenn Sabin, who writes about integrative health. Make sure your sources are current and that the therapies you choose have been proven based on scientific evidence. You can keep safe by discussing any alternative therapies with your medical team. For example, my nutritionist advised me to hold off on mushroom supplements during my chemotherapy since it might reduce its effectiveness.
- Get a second opinion from an academic cancer center, a cancer specialist, or online to confirm your diagnosis and your best treatment options. There are about 50 accredited cancer centers in the United States, including MD Anderson Cancer Center, the Cleveland Clinic, Dana-Farber Cancer Institute, Fred Hutch, Massachusetts General Hospital, the Mayo Clinic, Memorial Sloan Kettering, Stanford, and UCSF. Cancer specialists can be found online at services like Kyruus and ZocDoc. I introduce online services that can also provide recommendations on your best treatment options below.
The Revolution in Genetic Profiling and Personalized Molecular Therapies Creates a New Imperative: Determine Your List of 3–5 Treatment Options
Many, or most, people will respond to the standard treatment process for their cancer. For example, for a parent whose child has leukemia, the standard treatment has an 80%+ cure rate, so that’s almost always the appropriate path to take. In my case, the standard course of chemotherapy (“R-CHOP”) for follicular lymphoma has a 50% five-year progression-free survival rate. Encouraging people to explore other options probably isn’t helpful as it could delay starting appropriate treatment.
However, the exponential decrease in the cost of genetic analysis (sequencing) and explosive growth in new molecular cancer therapies means that someone with a cancer diagnosis needs to learn about and ensure access to the newest diagnostic tests and treatments. For example, new blood testing (“liquid biopsy”) for genetic profiling is emerging which will enable frequent, even continuous, monitoring. This may run against the grain for people who are like my father, who when diagnosed with stomach cancer got a hematologist he trusted and followed his guidance without question, or a friend who carried on her life with no change, not wanting to let the cancer define her. But bad things can happen if you don’t get involved:
- You can miss information and insights from genetic tests that can steer you to better treatment options. At most hospitals, you won’t get your tumor sequenced unless you ask.
- You can miss starting with new, less invasive life-saving options that are continuously being updated, e.g., clinical trials (experiments on humans), targeted therapies, off-label drugs. Instead, you will start with the standard of care: safe, tried and true, and optimized for the population, but usually with harmful side effects and possibly not personalized.
- You can pursue treatments that we know won’t work.
Doctors have for many years referred to someone’s cancer as being “in remission”, rather than “cured”, because cancer has a nasty way of mutating around treatments and coming back. This is particularly true of the newest cancer treatments (e.g., immunotherapy, CAR-T, TIL), which are less invasive than the traditional surgery, chemotherapy, or radiation, but because they are new, they only work for some people, or they work for a year or more, then the cancer returns. Therefore, the best approach is to always have a list of prioritized treatments, continuously updated, ready to try if your cancer returns. This means that when you get a cancer diagnosis you need to:
Step Three: Get your genomic data (via genomic profiling tests that sequence your tumor, healthy tissue, RNA, and microbiome) to gather information which will help you decide on your best treatment options. This is a step where you will need to advocate for yourself by asking for genomic diagnostic tests since only a few hospitals do it as a matter of course, and only a few insurance providers automatically pay for it. For an explanation of sequencing, please see the Sequence Me website, and for encouragement in how to ask for your tests see the Sequence Me “Battle Card”. You can choose to get your genetic tests through your healthcare provider, or there are dozens of diagnostic testing services, such as Foundation Medicine, Illumina, and Macrogen. (In a future article, I will describe how to choose from the 40+ companies I’ve identified that can capture your genetic data.)
Step Four: Analyze your data by making it available to services that will recommend your 3–5 best treatment options (such as surgery, chemotherapy, radiation, existing drugs, or clinical trials). This can be a second opinion at an accredited academic cancer center, or you can get it through one of many online service providers, such as Caris Life Sciences, CureMatch, Perthera, Sagely Health, and Tempus. (In another future article, I will recommend how to choose from the 40+ companies I’ve identified that offer advice on best treatment options.)
My Next Steps
When I met with my oncologist, he recommended that I get chemotherapy as fast as possible to shrink the mass that was causing my excruciating belly pain. I’ve completed the chemotherapy, the cancer is in remission, and I’m now looking at what I should do next. I have follicular lymphoma, a slow-growing cancer with a relatively high overall survival rate. However, follicular lymphoma is generally considered incurable. Roughly half of all follicular lymphoma patients eventually progress into a more aggressive lymphoma, which usually has a very poor prognosis. Therefore, I need to have my 3–5 best treatment options lined up.
Here’s what I’m doing to be actively engaged in my care, and what I recommend to anyone with a cancer diagnosis: First, I’m going to get my genetic data, including raw sequence data of sufficient depth and quality for my whole healthy cell genome, my whole cancer cell genome, my microbiome, and my cancer “transcriptome” (RNA) from sequencing services providers such as Illumina and Macrogen. And I’ve signed up for a clinical trial with a new blood biopsy company (Natera) to get personalized biomarkers to track my cancer’s progress. Second, I will release my data to several services providers (e.g., Sagely Health) that specialize in treatment recommendations, to get a variety of personalized treatment options.
Who knows what I will find? Hopefully there will be a therapy that is precise, with few toxic side effects, and support my native immune system. Right now, it seems like a personalized vaccine may be the best option. Stay tuned!
Disclaimer: In this article I have shared how I am thinking about my treatment, pushing the cutting edge of costly treatment steps that few people will be able to access and navigate. There is no guarantee that the diagnostic data I am going to get — and that I advocate that you get — will make a difference in treatment. And my approach is not intended to take the place of the recommendations of your trusted professional healthcare team; rather I offer it as some things to consider in your deliberations with them.
